Facilities providing medical or therapeutic care for individuals facing substance use disorders, mental health challenges, or co-occurring conditions within a specific city in Oregon constitute the core of behavioral health services available. These locations offer a range of programs, from detoxification and residential treatment to outpatient therapy and support groups. As an example, a person struggling with opioid addiction might seek assistance at a local clinic offering medication-assisted treatment.
Access to such local resources is crucial for community well-being. These specialized centers offer individuals opportunities for recovery, relapse prevention, and improved quality of life. Historically, access to care was limited, but the growth of dedicated centers has increased availability. The existence of accessible and effective treatment options reduces strain on local healthcare systems and contributes to a healthier, more productive society by addressing addiction and mental health problems directly.
The subsequent discussion will elaborate on the specific types of services offered by these centers, the methods of treatment employed, factors influencing choice of a treatment provider, and guidance on navigating the process of seeking help and accessing care locally.
Effective utilization of local addiction and mental health resources requires careful consideration of several key factors. This section outlines practical guidance to assist individuals and families in making informed decisions.
Tip 1: Assess Individual Needs: Prior to seeking assistance, it is crucial to determine the specific nature and severity of the presenting issues. A comprehensive assessment, potentially involving a medical professional, can help identify the appropriate level of care, whether it be outpatient therapy, intensive outpatient programming, or residential treatment.
Tip 2: Verify Credentials and Licensing: Ensure that any potential treatment facility possesses the required licenses and certifications from relevant regulatory bodies. Verification of staff credentials, including therapists and medical personnel, is also essential for quality assurance.
Tip 3: Inquire About Treatment Modalities: Different facilities may specialize in various treatment approaches, such as cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), medication-assisted treatment (MAT), or holistic therapies. Research the evidence-based practices employed by the facility and determine if they align with individual preferences and needs.
Tip 4: Understand Insurance Coverage and Payment Options: Clarify the extent to which insurance plans cover treatment services at the facility under consideration. Investigate payment options, including potential financing plans or scholarship opportunities, to address financial constraints.
Tip 5: Evaluate Facility Environment and Amenities: For residential programs, consider the physical environment of the facility. Factors such as cleanliness, safety, and the availability of amenities can impact the overall treatment experience. Visit the facility, if possible, or request a virtual tour.
Tip 6: Consider Aftercare Planning: A comprehensive treatment plan should include provisions for aftercare and relapse prevention. Inquire about the availability of ongoing therapy, support groups, and alumni programs to support long-term recovery.
Tip 7: Seek Referrals and Recommendations: Consult with primary care physicians, mental health professionals, or trusted sources for recommendations and referrals to reputable treatment facilities. Personal testimonials and online reviews can also provide valuable insights.
By carefully considering these factors, individuals can increase the likelihood of selecting a program that effectively addresses their specific needs and contributes to a successful recovery journey.
The subsequent sections will delve into resources and support systems available to assist in the navigation of local services.
1. Accessibility
Accessibility directly impacts the effectiveness of local behavioral health services. The easier it is for individuals to access assistance, the greater the likelihood of early intervention and improved outcomes. Factors influencing accessibility include the geographical distribution of facilities within the city, transportation options, wait times for appointments, and acceptance of various insurance plans. For example, a person residing in a rural area may face significant barriers to accessing care if the nearest treatment center is located a considerable distance away and public transportation is limited. This lack of physical access can delay treatment and exacerbate the underlying condition.
Another critical component of accessibility is affordability. Many individuals avoid seeking treatment due to concerns about cost, even if facilities are geographically accessible. When centers accept a wide range of insurance plans and offer sliding-scale payment options, more individuals can access the care they require. Beyond physical and financial considerations, cultural and linguistic accessibility are also vital. Facilities that provide services in multiple languages or offer culturally sensitive treatment approaches can better serve diverse communities. A real-world example is a center offering Spanish-speaking therapists, which removes a major barrier for the local Hispanic population needing assistance. Addressing all these dimensions of accessibility ensures equitable access to care.
In conclusion, the concept of accessibility is fundamental to the success of the behavioral health system. By prioritizing physical proximity, financial affordability, and cultural sensitivity, local facilities can maximize their impact and effectively serve the needs of the community. Failure to address these factors perpetuates disparities and limits the effectiveness of treatment efforts. Continued efforts to improve accessibility are essential for enhancing the well-being of individuals and the overall health of the community.
2. Specialized Programs
Within local treatment centers, specialized programs address the diverse needs of individuals seeking assistance. These programs tailor treatment approaches to specific demographics, disorders, or co-occurring conditions, enhancing the effectiveness of care.
- Substance-Specific Treatment
Facilities offer specialized programs targeted toward specific substances, such as opioids, alcohol, stimulants, or cannabis. For example, a local center might offer a medication-assisted treatment program specifically for individuals with opioid use disorder, employing medications like buprenorphine or naltrexone in conjunction with counseling and behavioral therapies. The focus is on managing withdrawal symptoms, preventing relapse, and providing education on the specific risks associated with the substance.
- Mental Health Specializations
Centers frequently provide specialized services for distinct mental health conditions, including anxiety disorders, depression, bipolar disorder, post-traumatic stress disorder (PTSD), and schizophrenia. An example is a program dedicated to treating PTSD in veterans, utilizing evidence-based therapies such as Cognitive Processing Therapy (CPT) or Eye Movement Desensitization and Reprocessing (EMDR). The program may also incorporate group therapy sessions and peer support to address the unique challenges faced by veterans with PTSD.
- Dual Diagnosis Programs
Recognizing the high co-occurrence of substance use disorders and mental health conditions, specialized dual diagnosis programs integrate treatment for both issues. A program addressing both conditions simultaneously, rather than treating them separately, may involve integrated therapy sessions, medication management, and skills-building activities designed to improve coping mechanisms and promote overall well-being. For instance, a client with both depression and alcohol use disorder would receive coordinated care addressing both conditions to prevent one from exacerbating the other.
- Age and Demographic Specific Programs
Programs can be tailored to meet the needs of specific age groups (adolescents, adults, seniors) or demographic groups (LGBTQ+ individuals, veterans, individuals with disabilities). A local example might be a program designed specifically for adolescents struggling with substance use and mental health issues, offering age-appropriate therapy, family counseling, and educational support. This tailored approach ensures that the unique challenges and developmental needs of adolescents are addressed effectively.
The presence of these specialized programs is a critical component of a comprehensive behavioral health system within the local setting. They represent an effort to provide targeted, evidence-based care that addresses the unique needs of individuals, thereby enhancing treatment outcomes and promoting long-term recovery. Without such specialization, the efficacy of the facilities in meeting the community’s diverse needs would be significantly compromised.
3. Licensing/Accreditation
Licensing and accreditation are fundamental components of reputable behavioral health services. These processes serve as indicators of quality and accountability within the field, particularly concerning centers offering assistance for substance use and mental health issues in this Oregon locale.
- State Licensing Requirements
State licensing establishes minimum standards for operation. Facilities must demonstrate compliance with regulations pertaining to safety, staffing, and service delivery. An example includes meeting specific staff-to-patient ratios to ensure adequate supervision and care. Non-compliance can result in fines, suspension, or revocation of the license, effectively prohibiting the center from operating. Licensing ensures a baseline level of consumer protection.
- Accreditation by Recognized Organizations
Accreditation, often voluntary, represents a higher level of quality assurance. Organizations such as The Joint Commission or the Commission on Accreditation of Rehabilitation Facilities (CARF) conduct rigorous evaluations of a facilitys policies, procedures, and outcomes. Achieving accreditation signifies a commitment to continuous improvement and adherence to industry best practices. A center accredited by CARF, for instance, has undergone a thorough review of its programs and services, demonstrating a dedication to providing high-quality, person-centered care.
- Impact on Insurance Reimbursement
Licensing and accreditation frequently influence insurance reimbursement rates. Many insurance providers require facilities to be licensed and/or accredited to be eligible for reimbursement. Without proper credentials, individuals may face higher out-of-pocket expenses, limiting access to care. For example, a center lacking accreditation may not be able to accept certain insurance plans, restricting services to those who can afford to pay privately.
- Public Trust and Confidence
Licensing and accreditation instill public trust and confidence in a facility’s ability to provide safe and effective care. These credentials serve as external validation of a center’s competence and commitment to ethical practices. Individuals seeking treatment are more likely to choose a licensed and accredited facility, believing it offers a higher level of quality and accountability. This trust is essential for fostering engagement in treatment and promoting successful outcomes.
The presence of valid licenses and accreditations offers a tangible assurance of quality within local treatment facilities. This validation ensures compliance with established standards and industry best practices, bolstering public trust and confidence in the provided care.
4. Treatment Modalities
The range of treatment modalities offered by local centers significantly impacts the effectiveness and suitability of care for individuals seeking assistance with substance use disorders and mental health conditions. The selection and implementation of these modalities are crucial for addressing diverse needs and promoting positive outcomes.
- Evidence-Based Therapies
These therapeutic approaches, validated through rigorous research, form the cornerstone of effective treatment. Cognitive Behavioral Therapy (CBT), for example, helps individuals identify and modify negative thought patterns and behaviors contributing to substance use or mental health challenges. Dialectical Behavior Therapy (DBT) teaches coping skills to manage intense emotions and improve interpersonal relationships. These therapies are often adapted to specific populations and disorders within local centers. For instance, a CBT program tailored for individuals with opioid use disorder might focus on relapse prevention strategies and coping with cravings. The integration of evidence-based therapies ensures that clients receive interventions with a proven track record of success.
- Medication-Assisted Treatment (MAT)
MAT combines pharmacological interventions with counseling and behavioral therapies to treat substance use disorders, particularly opioid and alcohol dependence. Medications such as buprenorphine, naltrexone, and methadone can reduce cravings and withdrawal symptoms, enabling individuals to engage more effectively in therapy and recovery. Local centers offering MAT must adhere to strict regulations and protocols, ensuring safe and responsible medication management. An example is the use of naltrexone injections to prevent relapse in individuals recovering from alcohol use disorder, allowing them to maintain abstinence while addressing underlying psychological issues.
- Group Therapy and Support Groups
Group therapy provides a supportive environment where individuals can share experiences, learn coping strategies, and build connections with others facing similar challenges. Facilitated by trained therapists, group sessions offer a sense of community and reduce feelings of isolation. Support groups, often led by peers in recovery, provide ongoing encouragement and guidance. Local centers may host various group therapy sessions, such as relapse prevention groups, anger management groups, or support groups for family members affected by addiction. These group settings foster empathy and promote mutual support, enhancing the overall treatment experience.
- Holistic and Complementary Therapies
Some centers incorporate holistic and complementary therapies to address the physical, emotional, and spiritual aspects of recovery. These approaches may include mindfulness meditation, yoga, art therapy, music therapy, or acupuncture. While not always considered evidence-based in the traditional sense, these therapies can enhance well-being, reduce stress, and promote relaxation. An example is the use of mindfulness meditation to help individuals manage anxiety and cravings, promoting a sense of inner peace and self-awareness. The integration of holistic therapies provides a more comprehensive and individualized approach to treatment.
The diverse array of treatment modalities available at local centers reflects a commitment to providing comprehensive and individualized care. By incorporating evidence-based therapies, medication-assisted treatment, group support, and holistic approaches, these facilities strive to address the multifaceted needs of individuals seeking recovery and improved mental health. The strategic selection and implementation of these modalities are essential for maximizing treatment effectiveness and fostering long-term success.
5. Insurance Coverage
Insurance coverage constitutes a critical determinant in accessing behavioral health services at local treatment centers. The extent and type of coverage significantly impact an individual’s ability to afford and receive necessary care for substance use disorders and mental health conditions within the designated locale.
- Plan Types and Network Affiliations
Various insurance plan types, including Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), and government-sponsored programs like Medicaid and Medicare, exhibit varying degrees of coverage for behavioral health services. A PPO plan, for example, might offer greater flexibility in choosing out-of-network providers, potentially expanding access to specialized programs not affiliated with an HMO. Conversely, an HMO may require referrals from primary care physicians, potentially delaying access to timely intervention. Treatment centers often maintain affiliations with specific insurance networks, influencing the range of plans they accept. Individuals must verify that their insurance plan is accepted by the desired treatment center to avoid unexpected out-of-pocket expenses. Understanding plan-specific details regarding network affiliations is crucial for navigating the landscape of available resources.
- Coverage for Specific Services
Insurance policies differ in their coverage of specific treatment modalities and services. Coverage for detoxification, residential treatment, intensive outpatient programs (IOPs), individual therapy, group therapy, and medication-assisted treatment (MAT) can vary significantly. Some plans may impose limitations on the duration of residential treatment or the number of therapy sessions covered per year. An individual seeking MAT for opioid addiction, for example, should verify that their insurance plan covers the specific medications prescribed, as well as the associated counseling and monitoring services. Thoroughly reviewing the policys coverage details ensures access to a comprehensive range of necessary services.
- Pre-Authorization Requirements and Utilization Review
Many insurance plans require pre-authorization for certain behavioral health services, particularly those involving higher levels of care, such as residential treatment or intensive outpatient programming. Pre-authorization involves obtaining approval from the insurance provider prior to initiating treatment. Utilization review, a process by which the insurance company assesses the medical necessity of ongoing treatment, may also be required. Failure to obtain pre-authorization or comply with utilization review requirements can result in denial of coverage. Centers must navigate these administrative processes to ensure clients obtain necessary approvals for treatment. Individuals should proactively communicate with their insurance provider and the treatment center to understand pre-authorization and utilization review requirements, minimizing potential disruptions in care.
- Mental Health Parity Laws
Federal and state mental health parity laws aim to ensure that insurance coverage for mental health and substance use disorders is comparable to coverage for physical health conditions. Parity laws prohibit insurance plans from imposing stricter limitations on mental health benefits, such as higher co-pays or fewer covered services. However, enforcement of parity laws remains a challenge, and some insurance plans may still exhibit subtle forms of discrimination. Individuals who believe their insurance plan is violating parity laws can file complaints with regulatory agencies. Mental health parity laws seek to promote equitable access to care for individuals with mental health and substance use disorders, reducing financial barriers to treatment.
In conclusion, insurance coverage plays a pivotal role in determining access to local treatment centers. Understanding the intricacies of plan types, coverage for specific services, pre-authorization requirements, and mental health parity laws is essential for navigating the complex landscape of behavioral health care. By advocating for comprehensive and equitable insurance coverage, individuals can increase their chances of receiving timely and effective treatment, promoting long-term recovery and improved well-being.
6. Aftercare Support
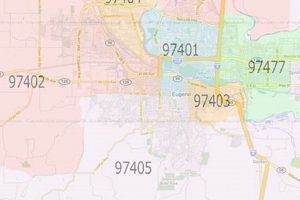
The period following primary treatment at facilities in the Eugene, Oregon area represents a critical phase in the recovery process. Aftercare support aims to sustain progress made during treatment and prevent relapse, ensuring individuals maintain their well-being and independence.
- Continued Therapy and Counseling
Ongoing individual or group therapy sessions provide a platform for individuals to address lingering issues, refine coping mechanisms, and navigate challenges encountered in daily life. For example, a person recovering from substance use may attend weekly therapy sessions to process triggers, develop relapse prevention strategies, and address underlying emotional issues that contributed to their addiction. These therapeutic interventions reinforce the skills learned during treatment and provide ongoing support for maintaining sobriety or managing mental health symptoms. In Eugene, local centers may offer specialized aftercare therapy programs, ensuring continuity of care.
- Support Groups and Peer Mentoring
Participation in support groups, such as Alcoholics Anonymous (AA), Narcotics Anonymous (NA), or mental health support groups, fosters a sense of community and shared experience. Peer mentoring programs connect individuals with experienced members of the recovery community who provide guidance, encouragement, and practical assistance. A person transitioning out of a residential treatment facility in Eugene may benefit from connecting with a peer mentor who has successfully navigated the challenges of early recovery in the local area. Support groups and peer mentoring programs offer valuable social support and reduce feelings of isolation, which can be particularly important during the vulnerable period following treatment.
- Relapse Prevention Planning
Developing and implementing a comprehensive relapse prevention plan is a crucial component of aftercare. This plan identifies potential triggers, coping strategies, and warning signs of relapse, equipping individuals with the tools to manage high-risk situations. A person with a history of relapse may work with a therapist to create a detailed plan that includes specific steps to take if they experience cravings or encounter triggering environments. In Eugene, aftercare programs may offer relapse prevention workshops or individual counseling sessions focused on developing personalized relapse prevention strategies. Regular review and adaptation of the relapse prevention plan ensures its continued relevance and effectiveness.
- Medication Management and Monitoring
For individuals receiving medication for mental health conditions or substance use disorders, ongoing medication management and monitoring are essential. This includes regular check-ups with a psychiatrist or medical provider to assess medication effectiveness, manage side effects, and ensure adherence to prescribed regimens. A person taking medication for depression, for example, would need ongoing monitoring to assess their mood, adjust medication dosages as needed, and address any potential side effects. Treatment facilities in Eugene collaborate with local medical providers to ensure seamless medication management and monitoring services for individuals in aftercare.
These facets of aftercare support represent a concerted effort to solidify gains achieved during formal treatment. By integrating continued therapy, peer support, relapse prevention strategies, and medication management, facilities in Eugene strive to enhance the long-term well-being and independence of those navigating recovery from substance use and mental health challenges.
7. Community Resources
Community resources are an integral component of comprehensive care provided by behavioral health facilities. The availability and effective integration of these resources significantly influence the success of treatment initiatives. Local support networks, housing assistance programs, vocational rehabilitation services, and peer-led organizations, act as extensions of formal treatment, facilitating a smoother transition for individuals into independent living. For example, a person completing a residential substance use program benefits substantially from immediate access to stable housing facilitated through a community partnership, reducing the risk of relapse triggered by homelessness or unstable living conditions. These resources contribute to a supportive ecosystem, reinforcing the principles of recovery and providing practical assistance to overcome obstacles encountered post-treatment.
The collaboration between treatment centers and community-based organizations creates a continuum of care, addressing multifaceted needs beyond clinical interventions. Vocational training programs, for instance, enhance employability and financial stability, mitigating stressors that contribute to substance use and mental health issues. Local food banks and clothing assistance programs alleviate basic needs insecurities, enabling individuals to focus on their recovery efforts without the added burden of survival-related anxieties. A person diagnosed with a mental health condition and exiting a local facility often benefits from referrals to peer support groups. These groups offer a sense of belonging, shared experiences, and strategies for managing daily challenges. The effectiveness of treatment is, therefore, contingent upon seamless connections to these various community assets.
In summary, community resources serve as vital adjuncts to treatment programs, addressing social determinants of health and enhancing the sustainability of recovery. The strength of these connections directly impacts the ability of individuals to successfully reintegrate into the community and maintain long-term well-being. Challenges exist in coordinating access to these diverse resources and ensuring equitable distribution, particularly for underserved populations. Strengthening the linkages between local facilities and community networks is essential to optimize treatment outcomes and foster a healthier, more resilient community.
Frequently Asked Questions About Localized Care
The following addresses common inquiries regarding options available for substance use disorders and mental health within the defined locale, offering concise and factual responses.
Question 1: What types of conditions are typically addressed by localized care facilities?
Facilities commonly address substance use disorders involving alcohol, opioids, stimulants, and other substances. Mental health conditions such as depression, anxiety, bipolar disorder, post-traumatic stress disorder (PTSD), and schizophrenia also constitute focal points of care. Dual diagnosis programs cater to individuals experiencing co-occurring substance use and mental health disorders.
Question 2: What treatment modalities are commonly employed?
Treatment modalities typically encompass evidence-based therapies like cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT). Medication-assisted treatment (MAT), group therapy, individual counseling, and holistic therapies may also be integrated into treatment plans.
Question 3: How does one verify the legitimacy and quality of a facility?
Verification involves confirming that the facility possesses valid state licenses and accreditations from recognized organizations such as The Joint Commission or CARF. Checking staff credentials and reviewing patient testimonials may further inform the assessment of quality.
Question 4: What are the typical costs associated with localized care, and are there financial assistance options?
Costs vary based on the type and duration of treatment. Insurance coverage, including private plans and government programs like Medicaid and Medicare, may cover a portion of the expenses. Facilities may offer sliding-scale fees, payment plans, or scholarship opportunities to mitigate financial barriers.
Question 5: What is the role of aftercare support in the recovery process?
Aftercare support encompasses continued therapy, support groups, peer mentoring, and relapse prevention planning. These components sustain progress made during initial treatment, promoting long-term recovery and preventing relapse.
Question 6: How can community resources enhance treatment outcomes?
Community resources, including housing assistance programs, vocational rehabilitation services, and peer-led organizations, provide practical support and facilitate reintegration into the community. These resources address social determinants of health, complementing clinical interventions and fostering sustained well-being.
Understanding these aspects facilitates informed decisions concerning behavioral healthcare.
The following discussion will transition to strategies for identifying the most appropriate facility.
Conclusion
The preceding discussion illuminated key aspects of localized facilities, detailing their accessibility, specialized programs, licensing standards, therapeutic modalities, insurance coverage dynamics, aftercare protocols, and integration with community support networks. It also addressed frequently asked questions to provide clarity for those seeking guidance. This examination sought to provide a comprehensive overview of the landscape.
Understanding the diverse facets of care, and options within treatment centers eugene oregon, individuals can make more informed decisions. Continued commitment to expanding access, enhancing quality, and fostering community collaboration is essential for improving outcomes. Prioritizing these considerations contributes to a healthier, more resilient community.